Abstract
Introduction: Multiple regulatory agencies and professional societies recommend risk assessment of hospitalized medical patients for hospital-acquired (HA) venous thromboembolism (VTE) and provision of pharmacologic prophylaxis to those at risk. Extant risk assessment models (RAMs) include risk factors not knowable or difficult to assess at admission and often do not include risk factors reflecting illness acuity (such as laboratory studies and vital signs at admission). We developed a RAM for HA-VTE that reports absolute VTE risk, as opposed to arbitrary risk categories, using only objective risk factors measured within the first 24 hours of admission.
Methods: The study setting was a combined academic and community 540-bed teaching hospital in northwest Vermont (The University of Vermont Medical Center). Using validated electronic health record (EHR) derived phenotypes (computable phenotypes), we captured all medical admissions between 2010-2019 and examined patient demographics, past medical history, and presenting vital and laboratory measures as potential risk factors for HA-VTE. As risk assessment should happen within 24 hours of admission, we only assessed risk factors knowable within this timeframe. Individuals with VTE at admission were excluded. Key outcome and risk factor definitions were validated using chart review. Bayesian logistic regression with a least absolute shrinkage and selection operator (LASSO) prior probability distribution was used to select risk factors for the model. Variables with a t-statistic ≥1.5 or ≤-1.5 were included in the final model. Full or prophylactic anticoagulation use was adjusted for in the final model. Model performance was assessed using bootstrap resampling to estimate area under the receiver operating characteristic (AUC) curve and calibration slope with 95% confidence interval (CI).
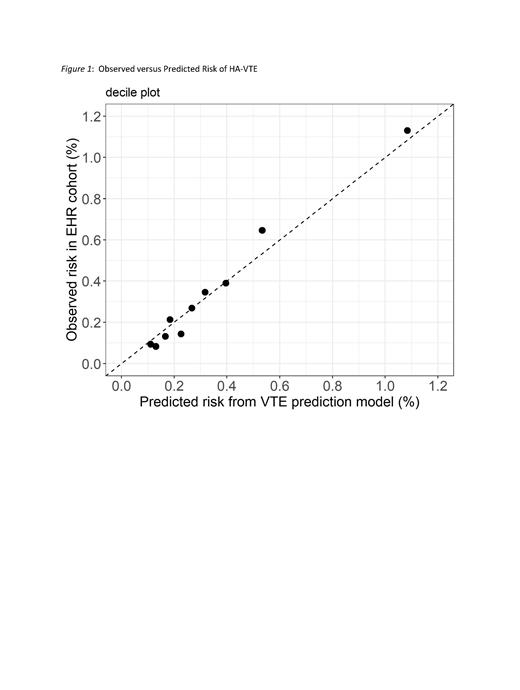
Results: There were 62,468 medical admissions in the study period with 219 HA-VTE events. Chart review demonstrated the positive predictive value of our HA-VTE computable phenotype to be 84% and the negative predictive value 99%. Mean age was 65 years and 51% were male. Comorbid conditions were common in this hospitalized population, including active cancer (29%), congestive heart failure (25%), diabetes (27%), hypertension (59%), and prior myocardial infarction (13%). Seven risk factors met the criteria for inclusion in the final model: prior history of VTE (OR 2.7; 95% CI 1.8, 3.8), red cell distribution width ≥14.7% (OR 1.6; 95% CI 1.2, 2.2), creatinine ≥2.0 mg/dL or on dialysis (OR 2.0; 95% CI 1.4, 2.8), serum sodium <136 MEq/L (OR 1.5; 95% CI 1.1, 2.1), active cancer (OR 1.4; 95% CI 1.1, 2.0), malnutrition based on prior reported weight loss (OR 2.1; 95% CI 1.3, 3.3), and low hemoglobin (<13.6 g/dL in men, <12.1 g/dL in women; OR 1.5; 95% CI 1.0, 2.1). The unadjusted AUC of the RAM was 0.73 with an unadjusted calibration slope 1.09 (Figure 1). The optimism-adjusted AUC was 0.68 (95% CI 0.64, 0.71) and the optimism-adjusted calibration slope was 0.87 (95% CI: 0.72, 1.03).
Discussion: We developed and internally validated a RAM for HA-VTE during medical hospitalization which incorporates simple, objective risk factors knowable within the first 24 hours of admission. Unlike most prior RAMs, this model also incorporates risk factors reflecting illness severity such as laboratory results. The RAM has good fit and calibration and will be moved forward to external validation. Future applications include incorporating the RAM into hospital admission workflows and assessing VTE prophylaxis rates and the incidence of HA-VTE and HA-bleeding.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal